之前放了教授鴿子
這次換教授放我鴿子
所以本來準備好一卡車資料要報告
卻陰錯陽差來聽了一場精采的演講..
剛好是我很有興趣的主題
也不管是不是會累得半死..就留下來聽了..
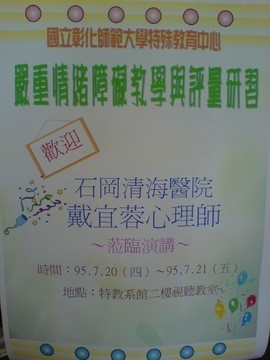
7/20 Selective Mutism, anxiety & depression
7/21 Selective Mutism, suicidal behavior...
先整理研習筆記
再打個人感想,又要動腦了..呼..真累..
不過心裡.腦裡得到很多東西..很爽!^^
***************************************************************************
研習筆記
1. DSM IV---
精神疾病診斷與統計手冊(The Diagnostic and Statistical Manual of Mental Disorders,簡稱為DSM)由美國精神醫學會(American Psychiatric Association,簡稱為APA)出版,是一本在美國與其他國家中最常使用來診斷精神疾病的指導手冊。
雖然這本手冊受到心理學家與精神病學家的廣泛接受,但是當中的精神疾病列表卻備受爭議。其中最有名的就是手冊第二版(簡稱為DSM-II)中將同性戀列為精神疾病的一種;這個條目在1973年由APA投票通過予以移除(請參看同性戀與心理學條目)。
DSM-I於1952年出版,當中列有60種不同的精神疾病。
DSM-II於1968年出版。
以上這兩版大量受到心理動力學方法的影響。所謂正常與非正常之間並沒有一個準確的區別,所有的精神疾病都被視為一種對環境事件的反應。精神疾病存在於一整個行為連續光譜之上。因此,每個人多多少少都有非正常的部份。那些不正常部份越嚴重的人,在功能運作上就擁有越多的困難。
前面幾版的DSM對精神病(psychosis)與精神官能症(neurosis)作了一個區分。精神病是一種嚴重的精神疾病,其特色為與現實脫離。精神病通常會有幻覺(hallucination)、妄想(delusion)與非邏輯性思考(illogical thinking)。精神官能症是一種比較輕微的精神疾病,其特色為將現實扭曲,但並沒有完全與現實脫離。精神官能症通常會有焦躁(anxiety)與憂鬱(depression)。
DSM-III於1980年出版,放棄了心理動力學觀點,改而使用一套醫療模式為主要診斷方法,使正常與不正常之間有了一個明確的區分。DSM變成了一個「非理論性」的手冊,因為它不探討精神疾病的成因。
第三版的修訂版(簡稱為DSM-III-R)於1987年出版。
DSM-IV 於1994年出版。
目前最新的版本為DSM-IV的修訂版,簡稱為DSM-IV-TR,於2000年出版。
第五版(簡稱為DSM-V)計畫是要到2010年才會出版。APA的研究部預期要到2005年或之後才會開始組成DSM的編輯工作小組。
然而, 它本身頗受爭議之處, 就是可以用投票方式決定疾病的存在與否(如1973年的同性戀), 並非如正統醫學以檢驗與病菌的方式做確認. 這樣渾沌混淆的診斷, 像憂鬱,躁鬱,過動等, 使精神病的治療更具不穩定性.
根據最新消息,最新一期《心理疾病與精神療法》雜誌上的調查說, 多數參與編撰手冊的專家與一些藥品製造商有著千絲萬縷的「曖昧」關係。在170名參與編撰1994年版《精神疾病診斷統計手冊》的專家中,有56%的人在1989-2004年間與至少一家制藥商有財務往來。並且這種財務關係花樣繁多,包括演講諮詢費、擁有公司股份、饋贈禮品、資助旅遊和研究。調查說,「這種令人生疑的關係在診斷領域的專家身上更為明顯,因為他們可以直接開出藥來。」
DSM IV的源起及特色何在?
大家一看到那個IV就知道,這本手冊已經修訂了四個版本。由於精神疾病是自古以來就存在的,而在西方從遠古時代將之視為鬼神附身、撒旦誘引…而將之視為「患者」予以治療及人性對待是在18世紀,而到了19世紀才有了所謂「心理健康」Mental Health的觀點,認為身體會生病而心理也一樣會生病。於是出現了許多在電視、電影上耳熟能詳的但不見得知道那是什麼的名詞如「精神分裂」、「多重人格」、「歇斯底里」…等等,這樣的觀念很好,然而出現了一個問題,那就是我們從喉嚨紅腫、發燒…等生理症狀可以來判定某人生了什麼病,所以有沒有可能也從患者的各種表現上來判定他是否患了某種精神疾病,於是有了第一本的DSM。有趣的是據說如果你去比較第一版及第四版,你很難相信那會是同一本書,可知精神疾病的定義是那樣的不確定及不容易。接下來我們來看看DSM IV有什麼特色:
以「操作型定義」來明確界定異常行為的類型,但也排除了許多無法被觀察到的可能原因。
從第三版到第四版改善了原先局限於個人行為因素,考慮了家庭、工作及社會環境的因素。
減少原先對精神患者在道德上的標籤作用,是疾患而非罪惡。
DSM IV是如何來診斷的?
在手冊的目錄部份將精神疾患分成16類(手冊p57-284)及可能為關注焦點的其他狀況(如親子、虐待…等),詳見手冊DSM IV分類表(p9-45):
1.通常初診斷於嬰兒期、兒童期或青春期的疾患 (智能不足、過動兒等)
2.譫妄、痴呆、失憶性疾患及其他認知疾患 (認知能力或記憶消失或速減)
3.一種一般性醫學狀況造成的精神疾患 (如由大腦受創所引起的)
4.物質關聯疾患 (酒精或藥物濫用等)
5.精神分裂及其他精神性疾患 (深信自己是蔣中正或常有幻聽或幻視)
6.情感性疾患 (不是指失戀哦!而是憂鬱症或躁鬱症情緒等)
7.焦慮性疾患 (萬分怕蟑螂、蛇等,恐懼症、懼曠症、社交恐懼症等)
8.身體型疾患 (總感覺這裡痛、那裡不對勁但看了好多醫生就是找不出病)
9.人為疾患 (故意製造或假裝造成的身體或心理的症狀)
10.解離性疾患 (大家最喜歡的多重人格、忘記自己是誰怎麼會來這裡等)
11.性疾患及性別認同疾患 (性功能障礙、戀童癖或曝露狂等)
12.飲食性疾患 (如木匠兄妹或宮澤理惠的心因性厭食症、暴食症等)
13.睡眠疾患 (走路走到一半突然睡著了的嗜睡症、夢遊等)
14.他處未分類之衝動控制疾患 (竊盜癖、縱火狂、病態性賭博及拔毛癖等)
15.適應性疾患 (受到壓力源所造成的無法適應等)
16.人格疾患 (反社會型、邊緣型、自戀型等人格)
以上有這麼多的疾患,那要如何來評定呢,手冊中每一項疾患都有不同數目的診斷標準(A,B,C…..)而有的診斷標準下又分許多的小項…等有的會註明在該項診斷標準下的5小項必有2個以上且持續多少時間以上才符合該診斷標準 ),而除非特別註明,否則滿足了每一項診斷標準(A,B,C…..)才能下診斷,想成為一名精神病患不是那麼容易的,是十分嚴格的。不要像我,還記得第一次翻DSM IV,怎麼隨便翻翻這個我也有、那條我也有,最後居然發現,整本書就好像我的日記,然後好幾天睡不著,那就十分傷腦筋了。
DSM IV的多軸向的評估系統
DSM IV是一個多軸向的評估系統Multiaxial Assessment,每一位精神患者的診斷都應包括五個軸向(詳見DSM IV手冊P.47-53),夠恐怖吧!其實也沒什麼啦,只是說治療者在以往治療精神疾患時,只考慮他的症狀,啊就常常治不好,所以把責任推給其它部份說「那是他家庭的因素、那是…」開玩笑的,而是精神疾病本來就根生理疾病不同,除了症狀及行為表現外,其家庭、系統等因素本來就十分的重要,用白話文講就是DSM IV現在嘗試從五個不同的層面及方向,來對患者做更整體的考量。接下來我們就來介紹有那五軸向:
第一軸向 臨床疾患、可能為臨床關注焦點的其它狀況大部份手冊中的精神疾患的診斷都放在這個軸向
第二軸向 人格疾患、智能不足比較因一個人發展上所出現的問題放在第二軸
第三軸向 一般性醫學狀況精神患者也可能有生理上的問題,不可不注意見手冊附錄G
第四軸向 心理社會及環境問題診斷這個人的支持系統、經濟、教育、法律、職業或犯罪等問題
第五軸向 功能整體評估從0-100分來評估,這個人的在自我、生活等整體功能好不好
也不一定對每一個患者都一定要五個軸的診斷,缺一個都不行,而只是如果有五個軸的話會有比較完整的了解。
如何來面對DSM IV?
DSM IV在學校是開成一門一學期的「臨床心理診斷」的課,要求之前必需修過「性格心理學」,所以並不是那麼的容易上手,而在下診斷的資格上則有更嚴格的要求,所以大家可以輕鬆的翻閱,對各類精神疾患的多樣性有一些概念,增加一些敏感度,都是很好的。
2. selective Mutism--
Selective mutism is a social anxiety condition, in which a person who is quite capable of speech, is unable to speak in given situations.
In the Diagnostic and Statistical Manual of Mental Disorders selective mutism is described as a rare psychological disorder in children. Children (and adults) with the disorder are fully capable of speech and understanding language, but fail to speak in certain social situations when it is expected of them. They function normally in other areas of behaviour and learning, though appear severely withdrawn and might be unwilling to participate in group activities. It is like an extreme form of shyness, but the intensity and duration distinguish it. As an example, a child may be completely silent at school, for years at a time, but speak quite freely or even excessively at home.
The disorder can also be the result of trauma experienced, especially at an early age, which gives such a shock and results in refusing to speak, which can then later lead to shyness of speaking especially if the child missed out on years of speech development.
The disorder is not regarded as a communication disorder, in that most children communicate through facial expressions, gestures, etc. In some cases, selective mutism is a symptom of a pervasive developmental disorder or a psychotic disorder.
In diagnosis, it can be easily confused with autistic spectrum disorder, or Aspergers, especially if the child acts particularly withdrawn around his or her psychologist. Unfortunately, this can lead to incorrect treatment.
Selective mutism is usually characterised by the following:
Consistent failure to speak in specific social situations (in which there is an expectation for speaking, e.g., at school) despite speaking in other situations.
The disturbance interferes with educational or occupational achievement or with social communication.
The duration of the disturbance is at least 1 month (not limited to the first month of school).
The failure to speak is not due to a lack of knowledge of, or comfort with, the spoken language required in the social situation.
The disturbance is not better accounted for by a Communication Disorder (e.g., Stuttering) and does not occur exlusively during the course of a Pervasive Developmental Disorder, Schizophrenia, or other Psychotic Disorder.
The former name elective mutism indicates a widespread misconception even among psychologists that selective mute people choose to be silent in certain situations, while the truth is that they are forced by their extreme anxiety to remain silent; despite their will to speak they just cannot make any voice. To reflect the involuntary nature of this disorder, its name has been changed to selective mutism in 1994. However, misconceptions still prevail; for instance, the ABC News erroneously attributed the cause of selective mutism to trauma and described it as willful in a report dated May 26, 2005.
The incidence of selective mutism is not certain. Owing to the poor understanding of the general public on this condition, many cases are undiagnosed. Based on the number of reported cases, the figure is commonly estimated to be 1 in 1000. However, in a 2002 study in The Journal of the American Academy of Child and Adolescent Psychiatry, the figure has increased to 7 in 1000.
No single cause has been established, but there is some evidence that there is a hereditary component and that it is also more common in girls than boys. Typical sufferers have some of the following traits when anxious, all of which are often perceived as rudeness:
They find it difficult to maintain eye contact. (anxiety)
Often don't smile and have blank expressions. (anxiety)
They move stiffly and awkwardly. (anxiety)
They find situations where talk is normally expected particularly hard to handle. Answering school registers, saying hello, goodbye, thank-you.
They tend to worry about things more than others
They can be very sensitive to noise and crowds
Find it difficult to talk about themselves or express their feelings
On the positive side, many sufferers have
Above average intelligence, perception, or are inquisitive
Are sensitive to others' thoughts and feelings (empathy)
Have very good powers of concentration (focused)
Often have a good sense of right/wrong/fairness (justice)
Treatment
Contrary to popular belief, people suffering from selective mutism do not necessarily improve with age, or just grow out of it. Consequently, treatment at an early age is important. If not addressed, selective mutism tends to be self-reinforcing, with the person being known as the one who doesn't speak which makes it all the harder to then speak. Sometimes in this situation, a change of environment (such as changing schools) to a place where the condition is not known can make the difference.
Occasionally, treatment in teenage years becomes more difficult, though not necessarily.
Forceful attempts to make the child talk are not productive, usually resulting in higher anxiety levels and so reinforcing the condition. The behaviour is often viewed externally as willful, or controlling, as the child usually shuts down all communication and body language in such situations, which is perceived as rudeness.
The exact treatment depends a lot on the subject, their age and other factors. Typically stimulus fading is used with younger children.
If anxiety medication is used it is needed at an extremely low dosage, higher doses may just make the problem worse
Stimulus Fading
In this technique the sufferer is brought into a controlled environment with someone who they are at ease with and can communicate. Gradually another person is introduced into the situation involving a number of small steps.
These steps are often done in separate stages in which case it is called the sliding-in technique, where a new person is slid into the talking group. This can take a relatively long time for the first one or two faded in people.
Desensitization
The subject is allowed to communicate via non-direct means to prepare them mentally for the next step. This might include email, phone, taped recordings, until they are in a position to try more direct communication.
Drug treatments
There is some evidence indicating that antidepressants such as fluoxetine may be effective in treating children with selective mutism, but only under closely controlled medical advice. These can sometimes decrease the anxiety levels enough to allow communication to take place.
See also
Autism
June and Jennifer Gibbons
Shyness
Social anxiety
Hikikomori
Other Organisations
SMIRA (Selective Mutism Information and Research Association) (UK)
3. anxiety--
Anxiety is a complex combination of negative emotions that includes fear, apprehension and worry, and is often accompanied by physical sensations such as palpitations, nausea, chest pain and/or shortness of breath.
Anxiety is often described as having cognitive, somatic, emotional, and behavioral components (Seligman, Walker & Rosenhan, 2001). The cognitive component entails expectation of a diffuse and uncertain danger. Somatically the body prepares the organism to deal with threat (known as an emergency reaction); blood pressure and heart rate are increased, sweating is increased, bloodflow to the major muscle groups is increased, and immune and digestive system functions are inhibited. Externally, somatic signs of anxiety may include pale skin, sweating, trembling, and pupillary dilation. Emotionally, anxiety causes a sense of dread or panic and physically causes nausea, and chills. Behaviorally, both voluntary and involuntary behaviors may arise directed at escaping or avoiding the source of anxiety. These behaviors are frequent and often maladaptive, being most extreme in anxiety disorders. However, anxiety is not always pathological or maladaptive: it is a common emotion along with fear, anger, sadness, and happiness, and it has a very important function in relation to survival.
Neural circuitry involving the amygdala and hippocampus is thought to underlie anxiety (Rosen & Schulkin, 1998). When confronted with unpleasant and potentially harmful stimuli such as foul odors or tastes, PET-scans show increased bloodflow in the amygdala (Zald & Pardo, 1997; Zald, Hagen & Pardo, 2002). In these studies, the participants also reported moderate anxiety. This might indicate that anxiety is a protective mechanism designed to prevent the organism from engaging in potentially harmful behaviors such as feeding on rotten food.
A chronically recurring case of anxiety that has a serious effect on a person's life may be clinically diagnosed as an anxiety disorder. The most common are generalized anxiety disorder, panic disorder, social anxiety disorder, phobias, obsessive-compulsive disorder, and posttraumatic stress disorder (一般焦慮症,恐慌症, 社會焦慮症, 恐懼症, 強迫症, 重鬱後症)
Diagnosis
A good assessment is essential for the initial diagnosis of an anxiety disorder, preferably using a standardized interview or questionnaire procedure alongside expert evaluation and the views of the person themselves. There should be a medical examination in order to identify possible medical conditions that can cause the symptoms of anxiety. A family history of anxiety disorders is suggestive of the possibility of an anxiety disorder.
Generalized anxiety disorder
Generalized anxiety disorder is a common chronic disorder that affects twice as many women as men and can lead to considerable impairment (Brawman-Mintzer & Lydiard, 1996, 1997). As the name implies, generalized anxiety disorder is characterized by long-lasting anxiety that is not focused on any particular object or situation. In other words it is unspecific or free-floating. People with this disorder feel afraid of something but are unable to articulate the specific fear. They fret constantly and have a hard time controlling their worries. Because of persistent muscle tension and autonomic fear reactions, they may develop headaches, heart palpitations, dizziness, and insomnia. These physical complaints, combined with the intense, long-term anxiety, make it difficult to cope with normal daily activities.
Panic disorder
In panic disorder, a person suffers brief attacks of intense terror and apprehension that cause trembling and shaking, dizziness, and difficulty breathing. One who is often plagued by sudden bouts of intense anxiety might be said to be afflicted by this disorder. The American Psychiatric Association (2000) defines a panic attack as fear or discomfort that arises abruptly and peaks in 10 minutes or less.
Although panic attacks sometimes seem to occur out of nowhere, they generally happen after frightening experiences, prolonged stress, or even exercise. Many people who have panic attacks (especially their first one) think they are having a heart attack and often end up at the doctor or ER. Even if the tests all come back normal the person will still worry, with the physical manifestations of anxiety only reinforcing their fear that something is wrong with their body. Extreme awareness of every little thing that happens or changes with their body can make for a stressful time.
Normal changes in heartbeat, such as when climbing a flight of stairs will be noticed by a panic sufferer and lead them to think something is wrong with their heart or they are about to have another panic attack. Some begin to worry excessively and even quit jobs or refuse to leave home to avoid future attacks. Panic disorder can be diagnosed when several apparently spontaneous attacks lead to a persistent concern about future attacks. A common complication of panic disorder is agoraphobia -- anxiety about being in a place or situation where escape is difficult or embarrassing (Craske, 2000; Gorman, 2000).
Phobia
This category involves a strong, irrational fear and avoidance of an object or situation. The person knows the fear is irrational, yet the anxiety remains. Phobic disorders differ from generalized anxiety disorders and panic disorders because there is a specific stimulus or situation that elicits a strong fear response. A person suffering from a phobia of spiders might feel so frightened by a spider that he or she would try to jump out of a speeding car to get away from one.
People with phobias have especially powerful imaginations, so they vividly anticipate terrifying consequences from encountering such feared objects as knives, bridges, blood, enclosed places, or certain animals. These individuals generally recognize that their fears are excessive and unreasonable but are generally unable to control their anxiety.
In addition to specific phobias, such as fears of knives, rats or spiders, there is another category of phobias known as social phobias. Individuals with this disorder experience intense fear of being negatively evaluated by others or of being publicly embarrassed because of impulsive acts. Almost everyone experiences "stage fright" when speaking or performing in front of a group. But people with social phobias become so anxious that performance is out of the question. In fact, their fear of public scrutiny and potential humiliaton becomes so pervasive that normal life can become impossible (den Boer 2000; Margolis & Swartz, 2001). Another social phobia is love-shyness, which most adversely affects certain men. Those afflicted find themselves unable to initiate intimate adult relationships (Gilmartin 1987).
Obsessive-compulsive disorder
Obsessive compulsive disorder is a type of anxiety disorder characterized by obsessions and/or compulsions. Obsessions are distressing, repetitive thoughts or images that the individual often realizes are senseless. Compulsions are repetitive behaviors that the person feels forced or compelled into doing, in order to relieve anxiety. One example would be the obsession of extreme cleanliness and fear of contamination, which may lead to the compulsion of having to wash one's hands hundreds of times a day. Another example may be the obsession that one's door is unlocked, which may lead to the constant checking and rechecking of doors.
Treatment overview
Mainstream treatment for anxiety consists of the prescription of anxiolytic agents and/or referral to a cognitive-behavioral therapist. There are indications that a combination of the two can be more effective than either one alone.
Prescription medication
The acute symptoms of anxiety are most often controlled with anxiolytic agents such as benzodiazepines. Diazepam (valium) was one of the first such drugs. Today there are a wide range of anti-anxiety agents that are based on benzodiazepines, although only two have been approved for panic attacks, Klonopin and Xanax. All benzodiazepines are physically addictive, and extended use should be carefully monitored by a physician, preferably a psychiatrist. It is very important that once placed on a regimen of regular benzodiazepine use, the user should not abruptly discontinue the medication.
Some of the SSRIs (selective serotonin reuptake inhibitors) have been used with varying degrees of success to treat patients with chronic anxiety, the best results seen with those who exhibit symptoms of clinical depression and non-specific anxiety or general anxiety disorder concurrently. Beta blockers are also sometimes used to treat the somatic symptoms associated with anxiety, especially the shakiness of "stage fright."
Many scientists believe that the benzodiazepines and other antianxiety drugs are greatly overprescribed and potentially addictive. See, for example, Fred Leavitt's The REAL Drug Abusers (Rowman & Littlefield, 2003). The addicitive nature of the benzodiazepine class became apparent in the mid 1960's when Valium (Diazepam), the first drug in the class to win FDA approval, resulted in thousands of people who quickly showed the classic symptoms of addiction when used for more than a week or two consistently.
The most addictive of the benzodiazepines appears to be Xanax due to its rapid onset and short half life in the blood stream. Xanax also has the dubious distinction of being the only benzodiazepine that often requires hospitalization for discontinuation as a precaution against dangerous and sometimes fatal seizures as part of the detoxification process. No other medications in this class have shown this fatal side effect, although abrupt discontinuation of virtually any benzodiazepine can result in cravings, stomach pains, cramps, increased anxiety, insomnia and other signs of withdrawal.
Cognitive-behavioral therapy (CBT) is the most popular and effective form of psychotherapy used to treat anxiety. The goal of the cognitive-behavioral therapist is to decrease avoidance behaviors and help the patient develop coping skills. This may entail:
Challenging false or self-defeating beliefs.
Developing a positive self-talk skill.
Developing negative thought replacement.
Systematic desensitization, also called exposure (used for agoraphobia and OCD mainly).
Providing knowledge that will help the patient cope. (For example, someone who suffers from panic may be informed that fast, prolonged, heart palpitations are in themselves harmless).
Unlike prescription medication, the effectiveness of cognitive-behavioral therapy depends on various subjective factors, such as therapist competence. In addition to conventional therapy, there are at-home cognitive-behavioral programs sufferers can use as part of their treatment.
Other coping strategies
A variety of over the counter supplements and medications are also used for their alleged anti-anxiety properties, however there is little scientific evidence to back up these claims. Kava Kava is a popular herbal treatment; small doses either taken regularly through the day or when early symptoms are noticed by the patient. Valerian root is also reputed to have anti-anxiety and sedative properties, as are passion fruit, passion flower, St. John's wort, hops, and chamomile.
Popular nutritional supplements for dealing with anxiety include magnesium and B-complex vitamins.
Self help and relaxation techniques also play an important role in relieving anxiety symptoms. Self help includes:
Proper diet - This includes reduction in consumption of caffeine, sugar, and generally an improvement of eating habits. Caffeine reduction should be gradual. Some anxiety sufferers report considerable reductions in their anxiety just from taking these measures.
Exercise - Some exercise is thought to relieve stress. Anxiety sufferers should note that rapid heart palpitations during exercise can trigger a panic attack, so it is probably better to gradually develop an exercise routine while on a cognitive-behavioral program.
Laughing
Breathing techniques and proper breathing - A Diaphragmatic breathing technique is often recommended (as opposed to chest breathing).
Proper sleep.
Meditation
Relaxation techniques - A state of relaxation can be achieved with the help of relaxation tapes, Yoga or relaxation therapy.
Stress management.- This may entail changes in lifestyle and time management. There are a number of books specialized in stress management.
Panic attack coping strategies - Specific strategies for dealing with panic episodes have been proposed, such as slow abdominal breathing and use of reassuring self-talk.
Search for meaning and purpose - Some experts have indicated that residual generalized anxiety can be the result of a sort of "boredom" about existence. They recommend looking for an occupation the sufferer finds meaningful.
For people who feel anxious and don't know why, it is worthwhile to sort out whether the anxiety is over a particular circumstance or a more abstract existential worry.
Alcoholic drinks are probably the most widely used substance for the alleviation of anxiety. Anxiety sufferers are cautioned that alcohol is also a powerful depressant and has a plethora of dangerous and uncomfortable side effects in addition to being potentially addictive. Some evidence suggests that consuming alcohol to alleviate anxiety may be counter-productive, as it can lead to a higher or irregular heartbeat and lowering of blood sugar which can both add to the unpleasant symptoms of anxiety and panic.
Anxiety in palliative care
Some research has strongly suggested that treating anxiety in cancer patients improves their quality of life. The treatment generally consists of counselling, relaxation techniques or pharmacologically with benzodiazepines.
Anxiety and alternative medicine
A 2002 CDC survey (see table 3 on page 9) found that complementary and alternative methods were used to treat anxiety/depression by 4.5 percent of U.S. adults who used CAM.
Existential anxiety
Theologians like Paul Tillich and psychologists like Sigmund Freud have characterized anxiety as the reaction to what Tillich called, "The trauma of nonbeing." That is, the human comes to realize that there is a point at which they might cease to be (die), and their encounter with reality becomes characterized by anxiety.
Religion, according to both Tillich and Freud, then becomes a carefully crafted coping mechanism in response to this anxiety since they redefine death as the end of only the corporal part of human personal existence, assuming an immortal soul. What then becomes of this soul and through what criteria is the cardinal difference of various religious faiths.
Philosophical ruminations are a part of this condition, and this is part of obsessive-compulsive disorder. They are typically about sex and religion or death.
According to Viktor Frankl, author of Man's Search for Meaning, when faced in extreme mortal dangers the very basic of all human wishes is to find a meaning of life to combat this "trauma of nonbeing" as death is near and to succumb to it (even by suicide) seems like a way out.
Test anxiety
Test anxiety is the uneasiness, apprehension, or nervousness felt by students who have a fear of failing an exam. Students suffering from test anxiety may experience any of the following: the association of grades with personal worth, embarrassment by a teacher, taking a class that is beyond their ability, fear of alienation from parents or friends, time pressures, or feeling a loss of control. Emotional, cognitive, behavioral, and physical components can all be present in test anxiety. Sweating, dizziness, headaches, racing heartbeats, nausea, fidgeting, and drumming on a desk are all common. An optimal level of arousal is necessary to best complete a task such as an exam; however, when the anxiety or level of arousal exceeds that optimum, it results in a decline in performance. Because test anxiety hinges on fear of negative evaluation, debate exists as to whether test anxiety is itself a unique anxiety disorder or whether it is a specific type of social phobia.
See also
Angst
Social Anxiety
General anxiety disorder

4. depression--
Clinical depression is a state of sadness, melancholia or despair that has advanced to the point of being disruptive to an individual's social functioning and/or activities of daily living. Although a low mood or state of dejection that does not affect functioning is often referred to as depression, clinical depression is a medical diagnosis and is different from the everyday meaning of "being depressed".
The diagnosis may be applied when an individual meets a sufficient number of the symptomatic criteria for the depression spectrum as suggested in the DSM-IV-TR or ICD-9/ICD-10. An individual is often seen to suffer from what is termed a "clinical depression" without fully meeting the various criteria advanced for a specific diagnosis on the depression spectrum. There is an ongoing debate regarding the relative importance of genetic or environmental factors, or gross brain problems versus psychosocial functioning.
Symptoms
According to the DSM-IV-TR criteria for diagnosing a major depressive disorder (cautionary statement) one of the following two elements must be present for a period of at least two weeks:
Depressed mood, or
Loss of interest or pleasure in nearly all activities.
It is sufficient to have either of these symptoms in conjunction with five of a list of other symptoms over a two-week period. These include:
Feelings of overwhelming sadness or fear or the seeming inability to feel emotion (emptiness).
A decrease in the amount of interest or pleasure in all, or almost all, activities of the day, nearly every day.
Changing appetite and marked weight gain or loss.
Disturbed sleep patterns, such as insomnia, loss of REM sleep, or excessive sleep (Hypersomnia).
Psychomotor agitation or retardation nearly everyday.
Fatigue, mental or physical, also loss of energy.
Feelings of guilt, helplessness, hopelessness, anxiety, or fear.
Trouble concentrating or making decisions or a generalized slowing and obtunding of cognition, including memory.
recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
Other symptoms sometimes reported but not usually taken into account in diagnosis include:
A decrease in self-esteem.
Inattention to personal hygiene.
Sensitivity to noise.
Physical aches and pains, and the belief these may be signs of serious illness.
Fear of 'going mad'.
Change in perception of time.
Depression in children is not as obvious as it is in adults. Here are some symptoms that children might display:
Loss of appetite.
Irritability.
Sleep problems, such as recurrent nightmares.
Learning or memory problems where none existed before.
Significant behavioral changes; such as withdrawal, social isolation, and aggression.
An additional indicator could be the excessive use of drugs or alcohol. Depressed adolescents are at particular risk of further destructive behaviors, such as eating disorders and self-harm.
One of the most widely used instruments for measuring depression severity is the Beck Depression Inventory, a 21-question multiple choice survey.
It is hard for people who have not experienced clinical depression, either personally or by regular exposure to people suffering it, to understand its emotional impact and severity, interpreting it instead as being similar to "having the blues" or "feeling down." As the list of symptoms above indicates, clinical depression is a serious, potentially lethal systemic disorder characterized by interlocking physical, affective, and cognitive symptoms that have consequences for function and survival well beyond sad or painful feelings.
Types of depression
The diagnostic category major depressive disorder appears in the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association. The term is generally not used in countries which instead use the ICD-10 system, but the diagnosis of depressive episode is very similar to an episode of major depression. Clinical depression also usually refers to acute or chronic depression severe enough to need treatment. Minor depression is a less-used term for a subclinical depression that does not meet criteria for major depression but where there are at least two symptoms present for two weeks.
Major clinical depression (重鬱症)
Major Depression, or, more properly, Major Depressive Disorder (MDD), is characterized by a severely depressed mood that persists for at least two weeks. Major Depressive Disorder is specified as either "a single episode" or "recurrent"; periods of depression may occur as discrete events or as recurrent over the lifespan. Episodes of major or clinical depression may be further divided into mild, major or severe. Where the patient has already had an episode of mania or markedly elevated mood, a diagnosis of bipolar disorder (also called bipolar affective disorder) is usually made instead of MDD; depression without periods of elation or mania is therefore sometimes referred to as unipolar depression because their mood remains on one pole. The diagnosis also usually excludes cases where the symptoms are a normal result of bereavement.
Diagnosticians recognize several possible subtypes of Major Depressive Disorder. ICD-10 does not specify a melancholic subtype, but does distinguish on presence or absence of psychosis.
Depression with Catatonic Features - This subtype can be applied to Major Depressive episodes as well as to manic episodes, though it is rare, and rarer in mania. Catatonia is characterized by motoric immobility evidenced by catalepsy or stupor. This MDD subtype may also manifest excessive, nonprompted motor activity (akathisia), extreme negativism or mutism, and peculiarities in movement, including stereotypical movements, prominent mannerisms, and prominent grimacing. There may also be evidence of echolalia or echopraxia. It is very rarely encountered, and may not be a useful category.
Depression with Melancholic Features - Melancholia is characterized by a loss of pleasure (anhedonia) in most or all activities, a failure of reactivity to pleasurable stimuli, a quality of depressed mood more pronounced than that of grief or loss, a worsening of symptoms in the morning hours, early morning waking, psychomotor retardation, anorexia (excessive weight loss, not to be confused with Anorexia Nervosa), or excessive guilt.
Depression with Atypical Features - Atypicality is characterized by mood reactivity (paradoxical anhedonia) and positivity, significant weight gain or increased appetite, excessive sleep or somnolence (hypersomnia), leaden paralysis, or significant social impairment as a consequence of hypersensitivity to perceived interpersonal rejection. People with this can react with interest or pleasure to some things, unlike most depressed individuals.
Depression with Psychotic Features - Some people with Major Depressive or Manic episode may experience psychotic features. They may be presented with hallucinations or delusions that are either mood-congruent (content coincident with depressive themes) or non-mood-congruent (content not coincident with depressive themes). It is clinically more common to encounter a delusional system as an adjunct to depression than to encounter hallucinations, whether visual or auditory.
Other categories of depression (低落性情感疾患)
Dysthymia is a long-term, mild depression that lasts for a minimum of two years. There must be persistent depressed mood continuously for at least two years. By definition the symptoms are not as severe as with Major Depression, although those with Dysthymia are vulnerable to co-occurring episodes of Major Depression. This disorder often begins in adolescence and crosses the lifespan. People who are diagnosed with major depressive episodes and dysthymic disorder are diagnosed with double depression. Dysthimic disorder develops first and then one or more major depressive episodes happen later.
Bipolar I Disorder is an episodic illness in which moods may cycle between mania and depression. In the United States, Bipolar Disorder was previously called Manic Depression. This term is no longer favored by the medical community, however, even though depression plays a much stronger (in terms of disability and potential for suicide) role in the disorder. "Manic Depression" is still often used in the nonmedical community.
Bipolar II Disorder is an episodic illness that is defined primarily by depression but evidences episodes of hypomania.
Postpartum Depression or Post-Natal Depression is clinical depression that occurs within two years of childbirth. Due to physical, mental and emotional exhaustion combined with sleep-deprivation; motherhood can "set women up" so to speak for clinical depression.
Premenstrual dysphoriais is a pattern of recurrent depressive symptoms tied to the menstrual cycle. The premenstrual decline in brain serotonin function is strongly correlated with the concomitant worsening of self-rated cardinal mood symptoms. Of considerable clinical importance, the recent understanding of premenstrual dysphoria as depression points directly to effective treatment with Selective serotonin reuptake inhibitor (SSRI) antidepressants. Previously, disrupting ovarian cyclicity had been the only recognized treatment. A recent review of studies of a number of SSRIs has revealed that they can effectively ameliorate symptoms of premenstrual dysphoria and may actually work best when taken only during the part of the menstrual cycle when dysphoric symptoms are evident. To that point, a study by Heim and Nemeroff et al., of Emory University, found that depressed and anxious women with a history of childhood abuse recorded higher heart rates and the stress hormone ACTH when subjected to stressful situations.
Hypomania(躁+鬱, bipola雙疾型疾患)
Hypomania, as the name suggests, is a state of mind or behavior that is "below" (hypo) mania. In other words, a person in a hypomanic state often displays behavior that has all the earmarks of a full-blown mania (e.g., marked elevation of mood that is characterized by euphoria, overactivity, disinhibition, impulsivity, a decreased need for sleep, hypersexuality), but these symptoms, though disruptive and seemingly out of character, are not so pronounced as to be considered a diagnosably manic episode.
Another important point is that hypomania is a diagnostic category that includes both anxiety and depression. It often presents as a state of anxiety that occurs in the context of a clinical depression. Patients in a hypomanic state often describe a sense of extreme generalized or specific anxiety, recurring panic attacks, night terrors, guilt, and agency (as it pertains to codependence and counterdependence). All of this happens while they are in a state of retarded or somnolent depression. This is the type of depression in which a person is lethargic and unable to move through life. The terms retarded and somnolent are shorthand for states of depression that include lethargy, hypersomnia, a lack of motivation, a collapse of ADLs (activities of daily living), and social withdrawal. This is similar to the shorthand used to describe an "agitated" or "akathitic" depression.
In considering the hypomania-depression connection, a distinction should be made between anxiety, panic, and stress. Anxiety is a physiological state that is caused by the sympathetic nervous system. Anxiety does not need an outside influence to occur. Panic is related to the "fight or flight" mechanism. It is a reaction, induced by an outside stimulus, and is a product of the sympathetic nervous system and the cerebral cortex. More plainly, panic is an anxiety state that we are thinking about. Finally, stress is a psychosocial reaction, influenced by how a person filters nonthreatening external events. This filtering is based on one's own ideas, assumptions, and expectations. Taken together, these ideas, assumptions, and expectations are called social constructionism.
On a final note, researchers at the University of California, San Diego, under the guidance of Hagop Akiskal MD, have found convincing evidence for the co-occurrence of hypomanic symptoms associated with a diagnosis of depression where the diagnosis does not meet criteria for Bipolar Disorder.[citation needed] Symptoms under consideration, such as irritability, misdirected anger, and compulsivity, also may not present sufficiently to be considered a hypomanic episode, as described by a Bipolar II Disorder. As noted in the Frank study [citation needed] mentioned above, this particular course of the disease, with the breakthrough of anxiety, may have a significant impact on the overall course of the depression.
This idea of co-occurring anxiety and depression is supported in a study by Giovanni Cassano MD of the University of Pisa and his collaborators on the Spectrum Project, who found a correlation between lifetime hypomanic and manic symptoms and the severity of the depression.[citation needed]
"The presence of a significant number of manic/hypomanic items in patients with recurrent unipolar depression seems to challenge the traditional unipolar-bipolar dichotomy."
These authors, along with many other researchers,[citation needed] argue in support of a revision of the approach to psychiatric diagnosis into what is being called the mood spectrum, so as to "[make] more accurate diagnostic evaluation[s]." This approach, although controversial, has begun to be given consideration by many behavioral health professionals.
Causes of depression
No specific cause for depression has been identified, but a number of factors are believed to be involved.
Heredity – The tendency to develop depression may be inherited; there is some evidence that this disorder may run in families. A 2004 press release from the National Institute of Mental Health declares "major depression is thought to be 40-70 percent heritable, but likely involves an interaction of several genes with environmental events."
Brain chemicals called neurotransmitters allow electrical signals to move from the axon of one nerve cell to the neuron of another. A shortage of neurotransmitters impairs brain communication.Physiology – There may be changes or imbalances in chemicals that transmit information in the brain, called neurotransmitters. Many modern antidepressant drugs increase levels of certain neurotransmitters, such as serotonin and norepinephrine. Although the causal relationship is unclear, it is known that antidepressant medications can relieve certain symptoms of depression, although critics point out that the relationship between serotonin, SSRIs, and depression usually is typically greatly oversimplified when presented to the public (see here). Recent research has suggested that there may be a link between depression and neurogenesis of the hippocampus. This horseshoe-shaped structure is a center for both mood and memory. Loss of neurons in the hippocampus is found in depression and correllates with impaired memory and dysthemic mood. The hippocampus regains mass when exposed to treatments that increase brain serotonin, and when regrown, mood and memory tend to be restored.
Seasonal affective disorder (SAD) is a type of depressive disorder that occurs in the winter when daylight hours are short. It is believed that the body's production of melatonin, which is produced at higher levels in the dark, plays a major part in the onset of SAD and that many sufferers respond well to bright light therapy, also known as phototherapy.
Psychological factors – Low self-esteem and self-defeating or distorted thinking are connected with depression. Although it is not clear which is the cause and which is the effect, it is known that depressed persons who are able to make corrections in their thinking patterns can show improved mood and self-esteem. Psychological factors related to depression include the complex development of one's personality and how one has learned to cope with external environmental factors such as stress.
Early experiences – Events such as the death of a parent, abandonment or rejection, neglect, chronic illness, and physical, psychological, or sexual abuse can also increase the likelihood of depression later in life. Post-traumatic stress disorder (PTSD) includes depression as one of its major symptoms.
Life experiences – Job loss, financial difficulties, long periods of unemployment, the loss of a spouse or other family member, divorce or the end of a committed relationship, or other traumatic events may trigger depression. Long-term stress at home, work, or school can also be involved. Bullying in late adolescence is also thought to be a contributing factor.
Medical conditions – Certain illnesses, including cardiovascular disease[9], hepatitis, mononucleosis, hypothyroidism, and organic brain damage caused by degenerative conditions such as Parkinson disease or by traumatic blunt force injury may contribute to depression, as may certain prescription drugs such as birth control pills and steroids. Gender dysphoria can also cause depression.
Diet – The increase in depression in industrialised societies has been linked to diet, particularly to reduced levels of omega-3 fatty acids in intensively farmed food and processed foods. This link has been at least partly validated by studies using dietary supplements in schools[and by a double-blind test in a prison. An excess of omega-6 fatty acids in the diet was shown to cause depression in rats.
Alcohol and other drugs – Alcohol can have a negative effect on mood, and misuse of alcohol, benzodiazepine-based tranquilizers, and sleeping medications can all play a major role in the length and severity of depression. The link between frequent cannabis use and depression is also widely documented, although the direction of causality remains in question; Dr. Salynn Boyles writes, ". . . research has linked pot smoking with depression and schizophrenia . . . daily use [of marijuana] was associated with a five-fold increase in later depression and anxiety among young women. But depression and anxiety were not predictive of later marijuana use."
Postpartum depression (also known as postnatal depression) – Dr. Ruta M Nonacs writes that while many women experience some mood changes after giving birth, "10-15% of women experience a more disabling and persistent form of mood disturbance (eg, postpartum depression, postpartum psychosis)." When it occurs, the onset typically is within three months after delivery, and it may last for several months. About two new mothers out of a thousand experience the more serious depressive disorder Postnatal Psychosis which includes hallucinations and/or delusions.
Living with a depressed person – Those living with someone suffering from depression experience increased anxiety and life disruption, increasing the possibility of also becoming depressed.[citation needed]
Social environment – Evolutionary theory suggests that depression is a protective mechanism: If an individual is involved in a lengthy fight for dominance of a social group and is clearly losing, depression causes the individual to back down and accept the submissive role. In doing so, the individual is protected from unnecessary harm. In this way, depression helps maintain a social hierarchy.
Other evolutionary theories – Another evolutionary theory is that the cognitive response that produces modern-day depression evolved as a mechanism that allows people to assess whether they are in pursuit of an unreachable goal. Still others claim that depression can be linked to perfectionism.
Recently some evolutionary biologists have begun to subscribe to the theory of "honest signalling". It has been pointed out that the incidence of major depression is much higher in persons born after 1945 which would seem to cast doubt on a possible disease model and that such suffering is notable in persons of greater than average intellect and emotional complexity. This contradicts the submission thesis.
Treatment
Treatment of depression varies broadly and is different for each individual. Various types and combinations of treatments may have to be tried. There are two primary modes of treatment, typically used in conjunction: medication and psychotherapy. A third treatment, electroconvulsive therapy (ECT), may be used when chemical treatment fails.
Other alternative treatments used for depression include exercise and the use of vitamins, herbs, or other nutritional supplements.
The effectiveness of treatment often depends on factors such as the amount of optimism and hope the sufferer is able to maintain, the control s/he has over stressors, the severity of symptoms, the amount of time the sufferer has been depressed, the results of previous treatments, and the degree of support of family, friends, and significant others.
Although treatment is generally effective, in some cases the condition does not respond. Treatment-resistant depression warrants a full assessment, which may lead to the addition of psychotherapy, higher medication dosages, changes of medication or combination therapy, a trial of ECT/electroshock, or even a change in the diagnosis, with subsequent treatment changes. Although this process helps many, some people's symptoms continue unabated.
In emergencies, psychiatric hospitalization is used simply to keep suicidal people safe until they cease to be dangers to themselves. Another treatment program is partial hospitalization, in which the patient sleeps at home but spends the day, either five or seven days a week, in a psychiatric hospital setting in intense treatment. This treatment usually involves group therapy, individual therapy, psychopharmacology, and academics (in child and adolescent programs).
Medication
Medication that relieves the symptoms of depression has been available for several decades. These drugs are listed in order of historical development. Typical first-line therapy for depression is the use of an SSRI, such as sertraline (Zoloft).
Monoamine oxidase inhibitors (MAOIs) such as Nardil may be used if other antidepressant medications are ineffective. Because there are potentially fatal interactions between this class of medication and certain foods and drugs, they are rarely prescribed anymore. MAOI's are used to block the enzyme monoamine oxidase which breaks down neurotransmitters such as serotonin and norepinephrine.MAOI's are as effective as tricyclics, if not slightly more effective. A new MAOI has recently been introduced. Moclobemide (Manerix), known as a reversible inhibitor of monoamine oxidase A (RIMA), follows a very specific chemical pathway and does not require a special diet.
Tricyclic antidepressants are the oldest and include such medications as amitriptyline and desipramine. Tricyclics block the reuptake of certain neurotransmitters such as norepinephrine and serotonin. They are used less commonly now because of their side effects, which include increased heart rate, drowsiness, dry mouth,constipation, urinary retention, blurred vision,dizziness, confusion, and sexual dysfunction. Most importantly, they have a high potential to be lethal in moderate overdose. However, tricyclic antidepressants are still used because of their high potency, especially in severe cases of clinical depression.
Selective serotonin reuptake inhibitors (SSRIs) are a family of antidepressant considered to be the current standard of drug treatment. It is thought that one cause of depression is an inadequate amount of serotonin, a chemical used in the brain to transmit signals between neurons. SSRIs are said to work by preventing the reabsorption of serotonin by the nerve cell, thus maintaining the levels the brain needs to function effectively, although two researchers recently demonstrated that this is a marketing technique rather than a scientific portrayal of how the drugs actually work. Recent research indicates that these drugs may interact with transcription factors known as "clock genes",which may be important for the addictive properties of drugs of abuse and possibly in obesity.
This family of drugs includes fluoxetine (Prozac), paroxetine (Paxil), escitalopram (Lexapro), citalopram (Celexa), and sertraline (Zoloft). These antidepressants typically have fewer adverse side effects than the tricyclics or the MAOIs, although such effects as drowsiness, dry mouth, nervousness, anxiety, insomnia, decreased appetite, and decreased ability to function sexually may occur. Some side effects may decrease as a person adjusts to the drug, but other side effects may be persistent.
Norepinephrine reuptake inhibitors such as reboxetine (Edronax) act via norepinephrine (also known as noradrenaline). NeRIs are thought to have a positive effect on concentration and motivation in particular.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine (Effexor) and duloxetine (Cymbalta) are a newer form of antidepressant that works on both noradrenaline and serotonin. They typically have similar side effects to the SSRIs, although there may be a withdrawal syndrome on discontinuation that may necessitate dosage tapering.
Dietary supplements
5-HTP supplements are claimed to provide more raw material to the body's natural serotonin production process. There is a reasonable indication that 5-HTP may not be effective for those who haven't already responded well to an SSRI.
S-adenosyl methionine (SAM-e) is a derivative of the amino acid methionine that is found throughout the human body, where it acts as a methyl donor and participates in other biochemical reactions. It is available as a prescription antidepressant in Europe and an over-the-counter dietary supplement in the United States. Clinical trials have shown SAM-e to be as effective as standard antidepressant medication, with many fewer side effects. Its mode of action is unknown.
Omega-3 fatty acids (found naturally in oily fish, flax seeds, hemp seeds, walnuts, and canola oil) have also been found to be effective when used as a dietary supplement (although only fish-based omega-3 fatty acids have shown antidepressant efficacy)
Dehydroepiandrosterone (DHEA), available as a supplement in the U.S., raises serotonin levels.
Chocolate improves mood, probably by raising serotonin.
Magnesium has gathered some attention
St John's Wort [Hypericum Perforatum] Traditionally used by 'wise women' and midwives for hundreds of years, to 'chase away the devil' of melancholia and anxiety. It is a mood-enhancing antidepressant supplement that increases the availability of serotonin, norepinephrine and dopamine at the neuron synapses. Also popular for treating insomnia, mood swings, fatigue, PMS and menopause.
Ginkgo Biloba Effective natural antidepressant said to stabilise cell membranes, inhibiting lipid breakdown and aiding cell use of oxygen and glucose - so subsequently a mental and vascular stimulant that improves neurotransmitter production. Also popular for treating mental concentration (such as for Alzheimer's and stroke patients).
Siberian Ginseng [Eleutherococcus Senticosus] Although not a true panax ginseng it is a mood enhancement supplment against stress. Also popular for treating depression, insomnia, moodiness, fatigue, poor memory, lack of focus, mental tension and endurance.
Zinc: 25mg per day have had an antidepressant effect in an experiment.
Biotin: a deficiency has caused a severe depression. The patient's symptoms improved after the deficiency was corrected.
The amino acids phenylalanine and tyrosine have also a favorable effect on easy forms of depression. They enhance the neurotransmitters dopamine and noradrenalin
Psychotherapy
In psychotherapy, or counseling, one receives assistance in understanding and resolving habits or problems that may be contributing to depression. This may be done individually or with a group and is conducted by health professionals such as psychiatrists, psychologists, social workers, or psychiatric nurses.
Effective psychotherapy may result in different habitual thinking and action which leads to a lower relapse rate than antidepressant drugs alone. Medication, however, may yield quicker results and be strongly indicated in a crisis. Medication and psychotherapy are generally complementary, and both may be used at the same time.
It is important to ask about potential therapists' training and approach; a very close bond often forms between practitioner and client, and it is important that the client feel understood by the clinician. Moreover, some approaches have been convincingly demonstrated to be much more effective in treating depression.
Counselors can help a person make changes in thinking patterns, deal with relationship problems, detect and deal with relapses, and understand the factors that contribute to depression.
There are many counseling approaches, but all are aimed at improving one's personal and interpersonal functioning. Cognitive behaviour therapy has been demonstrated in carefully controlled studies to be among the foremost of the recent wave of methods which achieve more rapid and lasting results than traditional "talk therapy" analysis. Cognitive therapy, often combined with behavioral therapy, focuses on how people think about themselves and their relationships. It helps depressed people learn to replace negative depressive thoughts with realistic ones, as well as develop more effective coping behaviors and skills. Therapy can be used to help a person develop or improve interpersonal skills in order to allow him or her to communicate more effectively and reduce stress. Interpersonal psychotherapy focuses on the social and interpersonal triggers that cause their depression. Narrative therapy gives attention to each person's "dominant story" by means of therapeutic conversations, which also may involve exploring unhelpful ideas and how they came to prominence. Possible social and cultural influences may be explored if the client deems it helpful. Behavioral therapy is based on the assumption that behaviors are learned. This type of therapy attempts to teach people more healthful types of behaviors. Supportive therapy encourages people to discuss their problems and provides them with emotional support. The focus is on sharing information, ideas, and strategies for coping with daily life. Family therapy helps people live together more harmoniously and undo patterns of destructive behavior.
如何幫助憂鬱症患者
▇ 有沒有這樣的朋友?
一、對各樣事情失去興趣,整天打不起勁
二、長期拒絕一般社交生活邀約,從朋友群中消失
三、中斷各種常態性的活動
四、突然冒出各種深奧、富哲理又偏向負面的話語
▇ 旁邊的人怎麼做?
一、帶他離開原來情境,前往就醫
二、儘量給予支持,讓他隨時有求助資源
5. suicidal behavior---
Suicide (from Latin sui caedere, to kill oneself) is the act of willfully ending one's own life. Suicide is sometimes used as a noun for one who has committed or attempted the act.
這是我最有興趣的議題..另打文作深入研究..

(這張照片三毛自己很喜歡)
想起她,就想起滄涼壯闊的自由、如風一般的愛情、水也似的笑容。她是少女時代珍貴的夢想和嚮往外面的世界的風景,開啟的窗是心靈最渴望的自由。
不能忘記夢裡花落知多少的刻骨銘心,沙漠上白手起家的情趣和對生活的熱愛。麻花辮的纯真、自來水加麵包走世界的灑脫、點一只烟背後的萬種風情。
世間的美女已經太多,紛紛擾擾的你方唱完我登場的秀色太容易得到也快失去印象。只有聰明的、靈秀的、善良的女子,才是世間最可貴的精采。

Seppuku (Japanese: 切腹, "stomach-cutting" or "belly slicing") is a form of Japanese ritual suicide by disembowelment. Seppuku is also known in English as hara-kiri (腹切り) and is written with the same kanji as seppuku but in reverse order with an okurigana. In Japanese, 'hara-kiri' is considered a somewhat vulgar term. The practice of committing seppuku at the death of one's master is known as oibara (追腹 or 追い腹) or junshi (殉死); the ritual is similar.
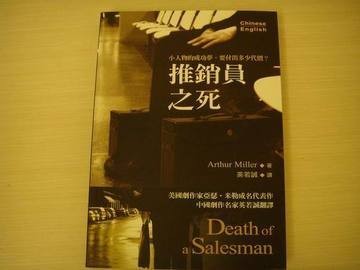
《推銷員之死》(Death of a Salesman ISBN 750010667X)是劇作家亞瑟·米勒的劇本,完成於1949年,是一部相當具有影響力的二十世紀戲劇。這部劇作被視為是一場對在資本主義下的美國夢相當嚴苛的批評,同時也讓米勒以及劇中主角「威利·羅曼」(Willy Loman)成為家喻戶曉的人物。《推銷員之死》在演出之後大受好評,贏得了1949年的普立茲獎,讓米勒成為美國的全國性作家。
劇情簡介
--->>>下文記有作品情節、結局或其他相關內容,可能降低欣賞原作時的興致。爆雷!
《推銷員之死》的主角威利·羅曼是一位逐漸在現實生活中失去事業能力的推銷員。威利的做事態度強調熱心誠懇以及交朋友的能力,他也一度聞名於整個新英格蘭,經常長時間開車四處兜售,他的兩個兒子畢甫(Biff)與哈比(Happy)讓他在鄰里間引以為傲,他的妻子琳達(Linda)則每天愉快的微笑。很不幸的,隨著時間過去,現在他的生活逐漸失去了控制。
威利已經辛苦工作了半生,而且應該要退休了,享受物質富裕的生活,並且在電話中不斷失去與過去的顧客之間的交易—特別是在一連串人格解體(depersonalization)與情境重現(flashback)等精神症狀後,他也失去了可以長途駕駛的能力。的確,威利曾經的努力似乎最後都失敗了:他被一個年紀可以當他兒子、而且是他當年欽點的後生晚輩炒了魷魚,而被迫要向之前的競爭同儕查理(Charley)貸款過活;他所有的老朋友與之前的顧客統統都不記得他了。而他34歲大的兒子,畢甫,並沒有跟上父親所走過的道路,而小兒子哈比總是成天無恥撒謊,假裝是一個完美的羅曼家子嗣。相反的,查理(威利曾經對他的兒子們說,這傢伙並不討人喜歡)卻成為了一位成功的生意人,而查理的兒子伯納德(Bernard),小時候是一位不耀眼的書蟲,長大後卻成為出色的律師。而因為威利在一次商務旅行中出軌,還讓畢甫失去了對他做為父親的信心。最後,威利還不斷被對他死去的兄長班(Ben)的回憶所糾纏,班曾經在早年前往阿拉斯加時說過:「…只要我能夠走到外頭,我就能變得有錢!」(And when I walked out, I was rich!)這句話不斷在他心頭縈繞,所以即使畢甫與哈比在家中束手無策,但是威利還是打算要找個方法,解決目前的困境。
這部劇作的結構使用了意識流的手法:威利不斷在他的客廳、下舞臺、前舞臺以及在虛幻的過去中,還有在想像中與班的對話中移動。米勒透過這些不同的狀態,更細膩、完整展現了威利的夢境以及在人生中的現實,以及讓角色出現在溫暖以及惡劣的燈光下,比較出角色的各種面向,最後鋪陳出整個完整的故事,不讓觀眾對任何角色做出某一種固定的評價。
最後問題的底層慢慢浮現了。威利相信、強調要成為受人喜歡的人,最後必能夠為他帶來完美的成功,而不是什麼困難的夢想,他一直保持著這樣的想法,而且決不放棄。他的兩個兒子不但受人喜歡,而且還相當英俊,而且就威利的角度來看,這樣的人格特質應該是人人都需要的。他以這樣的態度教導他的兒子,結果讓他的兩個兒子以為機運會自動降臨到他們身上。當然,現實生活並不是這麼的仁慈,兩個兒子最後都沒有辦法爭取機會,從事讓人尊敬的工作。威利發現了他自己與他兒子的失敗,於是更加緊了腳步,將希望放在他兒子的身上:他或許無法成功,但是兒子們或許可以;他的悲劇性缺點(tragic flaw)就是在他從不懷疑這樣的夢想是否有可能實現,哈比同樣對此毫不懷疑,他繼承了父親的態度,並且在第一幕的最後,遊說畢甫,要他要去貸款後可以快速致富。但是當畢甫嘗試去貸款的時候,他發現父親的缺點,他們在劇中互相叫罵:畢甫不斷指擇父親的精神疾病,威利則說畢甫只是在浪費生命、虛擲光陰並且傷了他的心。姑且不論這一場言詞戰爭對於他們的未來有何幫助,最後當畢甫打算放棄時,他含著眼淚說:「請你把那虛假的夢拿去燒掉,免得出事好嗎?」(Will you take that phony dream and burn it before something happens?)威利深受感動:因為畢甫仍然還是關心著他。
班突然出現在威利面前,和威利討論如果畢甫離家的話,到底能夠走得多遠,班說,畢甫可以先得到兩萬美元—那正是威利人壽保險上的數字。兩人說著說著進入狂喜,突然,鄰居都在一場爆炸聲中驚醒,而這爆炸聲正來自威利的車上:威利這位推銷員,以一種最莊嚴而且最荒謬的方式,用他的人生「換來」、而非是在他的人生中賺取得到家庭經濟的獨立。此刻,觀眾以及少數參與威利·羅曼喪禮的賓客,此時便不斷打量著他的墓丘,思索著他是一位怎樣的人,以及他的夢想,究竟值不值得。
劇中,處處可見人性的複雜及虛偽。父親在家人面前的自我膨脹,使兒
子在得知父親其實沒那麼偉大,甚至養小老婆之後,瀕臨崩潰而離家,開始
存著報復心態自暴自棄。然而,大兒子自己及小兒子其實在這樣的教育下,
一樣有說謊的習慣,裡外不一。看戲的我們,也只是無奈罷了,因為這是社
會導致的殘酷事實。
舞台的表現手法,在當時的眼光來看頗為有趣。現代的人物及威利的
想像人物交相出現,使觀眾知道現在的進行,又了解過去的種種。這樣技巧
的變化,給予這齣劇不同於小說的可看性。
亞瑟.米勒這部社會寫實經典名劇,描繪逐漸在現實生活中失去事業能力的推銷員威利?羅曼邁向死亡的歷程,藉小人物的悲劇,呈現資本主義下美國夢的幻滅。他運用意識流的手法,讓人物不斷在現實的情境、虛幻的過去及想像的對話中移動。
作者簡介
亞瑟.米勒(Arthur Miller, 1915-2005)
生長於紐約猶太中產階級家庭,美國經濟大蕭條時家道中落,中學畢業就自行工作謀生。後來就讀密西根大學新聞系,並開始從事劇本創作。1949年以劇作《推銷員之死》一舉贏得普立茲獎及紐約劇評人圈內獎,當時年僅卅三歲。米勒一生創作豐碩,被譽為「美國得獎最多的劇作家」。他的劇作與易卜生的寫實主義風格一脈相承,反映現實人生,著重探討家庭、道德和個人責任感。其他重要劇作有All My Sons(1947)、A Memory of Two Mondays(1955)、A View from the Bridge(1955)等。
萬維讀者網 2006-06-21 15:00:59
夢露前夫被FBI監視10余年
據京華時報報道, 美聯社在20日報道說,美國聯邦調查局在美國著名劇作家阿瑟‧米勒死後將他的檔案解密,根據這些檔案,這名曾與好萊塢銀幕偶像瑪麗蓮‧夢露成婚的劇作家,遭到聯邦調查局長達10余年的監視。
據報道,根據聯邦調查局的文件,曾寫出《推銷員之死》、《煉獄》等不朽名作的米勒在1944年首部劇本《鴻運高照的人》在百老匯上演後就被“盯上”,聯邦調查局對他進行了長達10余年的監視,直到1956年才結束。檔案中還包括匿名電話記錄,其中一個在米勒1956年與夢露成婚後的電話稱米勒是“共產黨員”,而夢露也在“向共產黨靠攏”。世界大戰後美國著名劇作家。因不滿麥卡錫主義,米勒1953年寫出《煉獄》,被譽為“美國戲劇的良心”。他還在1956年因拒絕回答非美活動調查委員會的提問被判處藐視國會罪。冷戰時期,聯邦調查局曾懷疑他是共產黨員。米勒2005年去世,享年89歲。
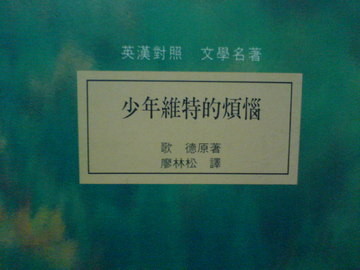
The nature of copycat suicides suggests that it is a phenomenon that must have been with us since the development of civilization. One of the earliest known associations between the media and suicide arose from Goethe’s novel Die Leiden des jungen Werthers (The Sorrows of Young Werther), published in 1774. In that work the hero shoots himself after an ill-fated love, and shortly after its publication there were many reports of young men using the same method to commit suicide. This resulted in a ban of the book in several places. Hence the term "Werther effect", used in the technical literature to designate copycat suicides.
全站熱搜


 留言列表
留言列表